Refracting the Achromatic Patient
"Doctors must adapt their testing methods to the achromat’s world, not make the achromat adapt to our bright clinical world. Only then, can we truly discover the individual’s potential vision."
- Richard L. Windsor, O.D., F.A.A.O.
Obtaining a precise measurement of the refractive error is important in all patients with decreased vision. Refraction, the measurement of the refractive  error (eyeglass prescription) and determination of visual acuity is much more complex in low vision patients and particularly in achromats. Special low vision refractive techniques are often required to obtain the most accurate eye wear prescription.
error (eyeglass prescription) and determination of visual acuity is much more complex in low vision patients and particularly in achromats. Special low vision refractive techniques are often required to obtain the most accurate eye wear prescription.
A careful low vision refraction may provide better visual acuity measurement and assure more effective and comfortable eyewear. We cannot afford to fail to provide the best visual acuity to patients with vision loss. The doctor providing the refraction should be experienced in low vision testing concepts including steps listed below.
Key Steps in Low Vision Refraction
Illumination of the room: The first step may be to reduce the room illumination, which may overwhelm the achromat and reduce their vision.
Illumination of the test chart: Our low vision examination rooms are designed to allow us to dim the lighting of the chart by rheostat to the level that the patient reports is comfortable. This will usually improve the comfort and responses of the achromat during refraction and frequently provides a better visual acuity. We must understand that this visual acuity is created under artificial control of the light. We recommend taking the visual acuity both with full light and at the preferred dimmer level of light. The disability determination measurements of vision are done under standard lighting test procedures.

Above, the room on the left shows normal lighting conditions. On the right, both the room and the chart light has been reduced to help the achromat function better. The patient indicates when the right light level is reached.
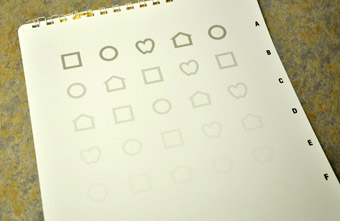
Training Young Children to the LEA Charts. Obtaining an accurate measurement 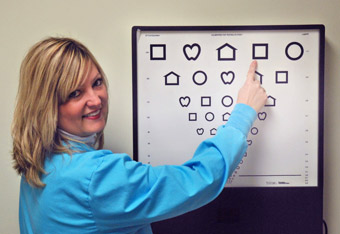 of visual acuity is critical in young achromats. Young children usually will not be able to read the standard test chart. With proper training and the use of LEA charts, however, many young children can learn to do the test accurately. It is often necessary to teach the child how to perform the test and identify the four symbols of the LEA charts. By 30 months, many children can learn to perform the test.
of visual acuity is critical in young achromats. Young children usually will not be able to read the standard test chart. With proper training and the use of LEA charts, however, many young children can learn to do the test accurately. It is often necessary to teach the child how to perform the test and identify the four symbols of the LEA charts. By 30 months, many children can learn to perform the test.
The LEA charts are an excellent way to accurately measure visual acuity in young children. The symbols can be used as wall charts or on separate handheld cards that allow good control of light and glare. This allows working with the child at a distance better for the child. See the charts below.

There are several ways to train the child to respond. The LEA symbols consist of four shapes: a square, a circle, a heart and a house. Thus the child who cannot read yet is only required to respond to four symbols. A copy of the four symbols can be used to allow the child to point to the correct shape.
A packet as shown below can be downloaded from the practice website to train with before the examination or sent home for the parents to use to train their child to respond to the 4 symbols. This can be used by the parents to help the child learn the four symbols which is then retested at the doctor's office.
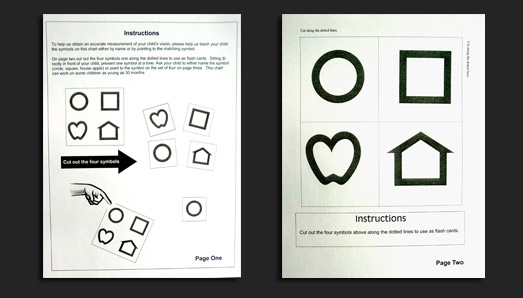
For other young children, the LEA puzzle can be used to teach the child how to recognize and respond to the four LEA symbols. See the puzzle below, which is first taught with the colored symbols as seen on the left then with the black and white, which on the other side which matches the test charts.
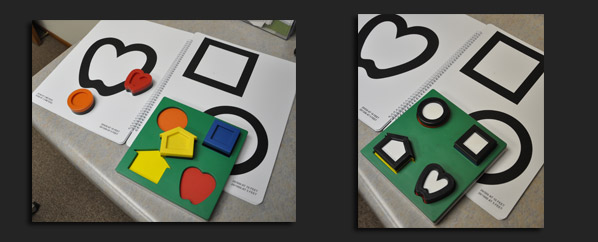
Once the child is able to do the LEA letters near vision and contrast sensitivity charts that use the LEA symbols can be used to test the child. The chart on the left below is a contrast sensitivity chart using LEA symbols.
 LEA Contrast Sensitivity Test
LEA Contrast Sensitivity Test
 Null positions: Nystagmus patient may have a null position, a head tilt or rotation of the head or eyes where the vision is best. This represents the position at which the nystagmus may slow providing slightly better visual acuity.
Null positions: Nystagmus patient may have a null position, a head tilt or rotation of the head or eyes where the vision is best. This represents the position at which the nystagmus may slow providing slightly better visual acuity.
Latent nystagmus: Latent nystagmus is an increase in the speed of movement of the eyes that occur when one eye is covered. Thus when we block one eye to take visual acuity or to measure the refractive prescription, we may reduce the patient’s measured visual acuity. If significant latent nystagmus is present, we may use a lens to blur the eye not being tested rather than a solid occluder.
Stress Induced Nystagmus: When individuals with nystagmus feel under stress, it is not uncommon for the nystagmus to increase. It is critical that we reduce stress and take our time to let the patient feel comfortable during the refraction.  Larger Refractive Steps: Basic low vision techniques may include demonstrating larger changes in the lenses. Rather than .25 diopter steps, the low vision doctor may use 1.00 diopter changes as needed.
Larger Refractive Steps: Basic low vision techniques may include demonstrating larger changes in the lenses. Rather than .25 diopter steps, the low vision doctor may use 1.00 diopter changes as needed.
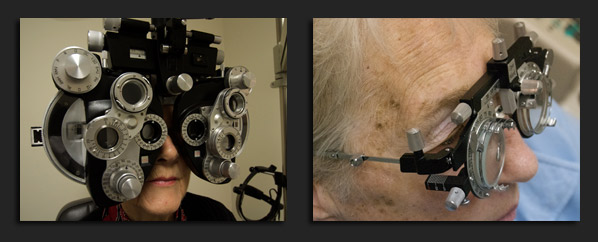
The use of stronger (1.00 diopter) cross cylinder test pieces to test for astigmatism as shown on the left. These increase the amount of change the patient sees when the doctor asks which is better one or two.
Here a trial frame is used with a cross cylinder to determine the power and position of the astigmatism. The patient is able to see a larger difference in the change.

Eccentric Fixation: Patients may turn their eyes or head slightly not only because of the nystagmus, but also owing to a need to move the image slightly to the side of the macula. This is present less in achromatopsia, but it does occur in those with the lower levels of vision. The phoropter as shown on the left below is used whenever possible but it limits the ability of the patient to shift their eyes to eccentrically fixate or to move to the null position of best vision in nystagmus. Using a trial frame as shown on the right below, with hand held lenses allows the patient to move their eyes and head as needed and thus may provide a more accurate test.
Testing Through Filters: In achromats, it may be helpful to test the refraction with filters in place or through plano or non-powered filtered contact lenses.

Objective Testing Methods: Because of the high amount of hyperopia or farsightedness in many rod monochromats, a cycloplegic refraction should be initially considered on young  children. The medication used will relax the child’s focusing ability and help detect higher amounts of hyperopia than found on standard refraction. Using cycloplegic refraction with retinoscopy in very small children, allows measurement of their refractive error without requiring the child to respond.
children. The medication used will relax the child’s focusing ability and help detect higher amounts of hyperopia than found on standard refraction. Using cycloplegic refraction with retinoscopy in very small children, allows measurement of their refractive error without requiring the child to respond.
Autorefractors, equipment that scans the eye automatically and determines the refractive error, can be very helpful in children and adults.
 Autorefractor
Autorefractor
Educating the Patient: Highly hyperopic patients need instruction on the parallax motion of high plus lenses and how contacts eliminate this motion effect. When the patient’s eyes move across the highly farsighted lenses, the world will seem to stream quickly in the opposite direction. This can be very uncomfortable and a reason that some achromats reject wearing their eyewear.
Contact lenses can solve this problem, because as the eye moves the contact lens moves with the eye keeping the optical center of the lens always in the same position. Thus the contact lenses cause no parallax movement of the world.
Reducing the power can also reduce the speed of the movement. In some cases, prescribing a lower power may be more wearable.
Testing for Bifocals: Bifocals need to be considered by school age or sooner. The amount of accommodation or focusing required at a very close distance can eventually fatigue even young children who have high amounts of focusing ability. Those doctors not experienced in low vision may not anticipate the value of a bifocal for the child achromat. Today, we can prescribe very strong invisible bifocals up to +7.00 diopters of power. Convergence and Phoria Testing: Patients with poor ocular convergence or other eye muscle imbalances may have difficulty sustaining the close distances required to read with achromatopsia.
Convergence and Phoria Testing: Patients with poor ocular convergence or other eye muscle imbalances may have difficulty sustaining the close distances required to read with achromatopsia.
The closer reading distance required of most achromats puts more demand on the ability to converge the eyes together. Adding prism may improve comfort. Many forms of reading eyewear have built-in prism to improve convergence.
 Test Computer Vision: Computers are becoming critical in nearly everyone's life. The ability to sustain clear comfortable vision at the computer should be tested.
Test Computer Vision: Computers are becoming critical in nearly everyone's life. The ability to sustain clear comfortable vision at the computer should be tested.
Focus is based on the distance to the reading material or computer. The distance to the computer screen is different from the distance at which most individuals read. In fact most achromats read at a very close distance.
If they wear bifocals or have reading eyewear, they are usually based on a very close reading distance to produce angular magnification. This often creates problems at the computer, since neither the distance portion of their eyewear nor the bifocals or reading eyewear may focus properly at the distance to the computer screen. This should be tested during the examination. Filter levels should be tested for viewing a real computer screen and antireflection coating prescribed to reduce glare. The doctor should consult with the patient on positioning of the computer, use of larger monitors, screen magnifiers and control of lighting around the computer monitor. Avoid bright surfaces or windows behind the computer.